Expanding Federal Work Requirements for Medicaid Expansion Coverage to Age 64 Would Increase Coverage Losses
By Michael Karpman, Jennifer M. Haley, Genevieve M. Kenney / April 30, 2025
National and State Estimates for Adults Ages 19 to 64
This analysis examines potential Medicaid coverage losses in 2026 under a federal Medicaid work requirement for adults ages 19 to 64 enrolled in the Affordable Care Act’s expansion. It builds on our estimates of coverage losses at the national and state levels under a federal Medicaid work requirement for expansion enrollees. Our previous estimates applied to enrollees ages 19 to 55 and showed that 4.6 to 5.2 million adults ages 19 to 55 would lose Medicaid coverage under a policy similar to the Limit, Save, Grow Act of 2023 if experiences followed those in two states with prior work requirements in Medicaid.
This analysis finds that extending work requirements up to age 64 would result in an additional loss of federally funded Medicaid coverage for approximately 1 million adults. Overall, an estimated 5.5 to 6.3 million expansion enrollees ages 19 to 64—or 36 to 42 percent of expansion enrollees in this age range—would lose eligibility for federally funded Medicaid coverage in 2026 under federal work requirements.
An Estimated 5.6 to 6.3 Million Adults Would Lose Coverage If Medicaid Work Requirements Are Extended to All Expansion Enrollees Ages 19 to 64
The numbers of affected enrollees and potential coverage losses would be higher if Medicaid work requirements were extended to include expansion enrollees up to age 64.
About 1.8 million more adults would be subject to work requirements that apply up to age 64 compared with work requirements that apply up to age 55. We project that an additional 1 million adults would lose federally funded Medicaid coverage in 2026 under work requirements that extend up to age 64 (5.5 to 6.3 million under a policy that extends to age 64 versus 4.6 to 5.2 million under a policy that extends to age 55).
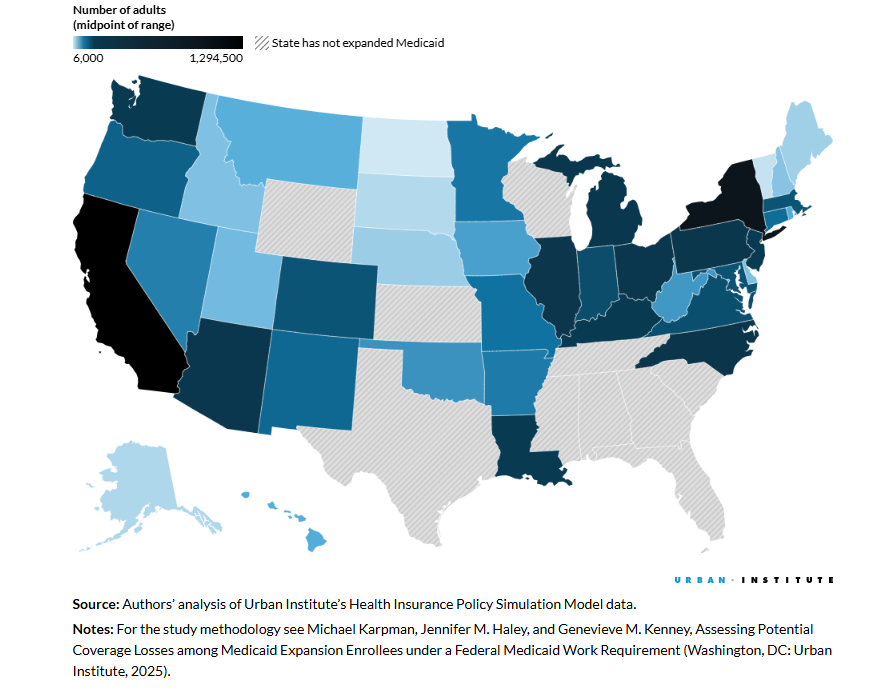
Coverage losses would be higher in every state if Medicaid work requirements extend to age 64 rather than 55, and more states would have enrollment losses of over 100,000 in 2026.
Whether work requirements extend to age 55 or age 64, at least 10,000 adults in almost every Medicaid expansion state would lose coverage, with variation across states reflecting the number and composition of expansion enrollees. Under work requirements that apply up to age 64, 17 states would see coverage losses of more than 100,000—up from 13 states under a policy that extends to age 55.
Most expansion enrollees who would be subject to work requirements—whether they extend to age 55 or 64—are already engaged in work activities or could meet exemption criteria.
Our analysis finds that about half of all expansion enrollees in both age groups could be automatically exempted from work requirements based on parental status, earning wages consistent with working 80 hours per month based on the federal minimum wage, or complying with Supplemental Nutrition Assistance Program work rules. Among the remainder who would be subject to work requirements and do not have one of the characteristics that we assume states could use to automatically exempt them from the requirements, more than three-quarters are working some or all months of the year, attending school, looking for a job, caring for a disabled household member, or are in fair or poor health or have a functional limitation (81 percent of expansion enrollees ages 19 to 55 and 78 percent of those ages 19 to 64).
Overall, about 9 in 10 enrollees in both age groups participate in work-related activities or have observable characteristics that could qualify them for an exemption (91 percent of expansion enrollees ages 19 to 55 and 89 percent of those ages 19 to 64).